Selection of videos for Snoring & Obstructive Sleep Apnoea
Overview of Snoring & Obstructive Sleep Apnoea
This is simply an overview of Snoring & Obstructive Sleep Apnoea.
Understanding Sleep Disordered Breathing
What is Sleep Disordered Breathing?
If you wake up exhausted after a full night in bed, or your partner regularly complains about your snoring, you may be experiencing Sleep Disordered Breathing (SDB). This encompasses a range of conditions from simple snoring through to Obstructive Sleep Apnoea (OSA), all of which disrupt normal breathing during sleep and can significantly affect the quality of rest for both you and your bed partner.
What Causes Snoring and Sleep Disordered Breathing?
Loud snoring is one of the most common symptoms of Sleep Disordered Breathing. The noise typically originates in the throat, caused by vibrations of the soft tissues as air passes through a narrowed airway. Despite how common it is, the underlying mechanisms and effective treatments can be surprisingly complex.
Many medical professionals, including ENT surgeons, often lack specific training in this specialised area of sleep medicine. Prof Vik Veer is one of the few surgeons in the country employed by the NHS specifically to treat Sleep Disordered Breathing, bringing expertise that remains relatively rare in the UK.
"After having complaints for many years related to my sleep apnoea and told there was nothing wrong with me or they simply didn't know what to do by other healthcare professionals, Professor Veer immediately understood everything about all my symptoms and had immediate advice on next steps to improve my condition."
– True Google review
The Sleep Disordered Breathing Spectrum: Where Do You Fall?
Sleep Disordered Breathing exists on a spectrum, ranging from simple snoring at one end to severe Obstructive Sleep Apnoea at the other. Understanding where you fall on this spectrum is important for seeking appropriate treatment.
Simple Snoring
Approximately 42% of middle-aged men snore regularly. Whilst this can be disruptive, it isn't always indicative of a more serious underlying issue. That said, it's worth investigating if it's affecting your quality of life or relationships.
Obstructive Sleep Apnoea (OSA)
Affecting roughly 4% of the population, OSA is characterised by repeated episodes of complete or partial obstruction of the airway during sleep. This results in temporary cessation of breathing (apnoea) or shallow breathing (hypopnoea). The concerning aspect is that many people with OSA are entirely unaware they have it, despite the condition having potentially serious consequences if left untreated.
Upper Airways Resistance Syndrome (UARS)
UARS sits between snoring and sleep apnoea on the spectrum. Rather than complete obstruction, you experience increased resistance to airflow in the upper airways. This results in laboured breathing, often producing a deep breathing noise rather than typical snoring or silence. UARS can cause significant discomfort and symptoms similar to OSA, including daytime fatigue and disrupted sleep. Prof Vik Veer considers UARS worthy of recognition as a distinct condition due to its unique characteristics and impact on wellbeing.
Obesity Hypoventilation Syndrome (OHS)
This breathing disorder affects individuals with severe obesity. Essentially, there is too much weight pressing down on the chest at night, resulting in an inability to take adequate breaths. This is characterised by inadequate ventilation, leading to elevated blood carbon dioxide levels and reduced oxygen levels.
"It was wonderful to finally have confirmation that I do have a sleep disorder and that action is necessary! I now feel confident that Mr Veer can improve my sleep and, as a result, improve my life."
– Felicity Knapton, Google review
The Real Impact of Sleep Apnoea
Individuals with OSA experience multiple episodes of airway obstruction during sleep, leading to frequent partial awakenings. These interruptions can occur more than five times an hour, significantly disrupting the sleep cycle and leading to chronic fatigue. In severe cases, individuals may partially wake more than once a minute throughout the night.
The lack of restful sleep has wide-ranging effects on overall health. Untreated sleep apnoea is associated with cardiovascular disease, cognitive impairment, diabetes, high blood pressure, and a marked decrease in quality of life. These aren't simply inconveniences; they represent serious long-term health risks that can reduce life expectancy by approximately 20 years.
Symptoms of Sleep Apnoea: What to Look For

There are surprisingly few obvious symptoms of Obstructive Sleep Apnoea, which makes the condition rather difficult to identify. Most people have no recollection of the breathing interruptions happening at night. Some can stop breathing every 30 seconds, experiencing dangerous drops in oxygen levels, whilst having absolutely no awareness of it.
The symptoms below may indicate sleep apnoea:
- Waking unrefreshed
You've been in bed for eight hours, but you feel like you've hardly slept at all. This happens because you're being partially woken up multiple times every hour throughout the night, completely unaware in the vast majority of cases. Imagine someone prodding you awake every few minutes all night long. You never get into the deep, restorative sleep your body needs to recover and feel refreshed. - Never getting a good night's sleep
Even on nights when you think you've slept well, you haven't. Your brain never gets the chance to cycle properly through all the sleep stages it needs. You're stuck in light sleep, constantly being interrupted by your body's desperate attempts to restart your breathing. - Daytime tiredness and nodding off
Falling asleep during meetings, whilst watching television, or even whilst driving. This isn't normal tiredness from a busy day. This is your body trying to make up for months or years of severely disrupted sleep. The sleep debt builds up, and your body will try to claim it back whenever it can, often at dangerous moments. - Mental fog and difficulty concentrating
You know that feeling when you're trying to focus but your brain just won't cooperate? Sleep apnoea robs you of REM sleep (dream sleep), which is when your brain consolidates memories and processes information from the day. Without enough REM sleep, your ability to concentrate, remember things, and think clearly all suffer. Simple tasks feel harder than they should. This is why 40% of car accidents in this country are caused by someone with obstructive sleep apnoea. - Waking gasping or choking
Some apnoea episodes are so severe that your body forces you to fully wake up, gasping for air. This can be terrifying, both for you and for anyone sleeping beside you. Your oxygen levels have dropped so low that your brain has no choice but to jolt you awake to prevent further harm. - Waking multiple times to urinate
You might assume this is a bladder or prostate problem, but the real cause is often sleep apnoea. Here's why: a hormone called atrial natriuretic peptide (ANP) is released from your heart, which normally helps stop your bladder from filling up at night. In the morning, your kidneys start clearing themselves out and your bladder fills normally. The problem with sleep apnoea is that your body is constantly being woken up, so it keeps thinking it's morning. Your body is tricked into filling up the bladder repeatedly throughout the night. Many people undergo unnecessary tests or treatments for bladder problems when fixing their sleep apnoea would solve the issue entirely. - Night sweats
Your sympathetic nervous system (your body's "fight or flight" response) goes into overdrive throughout the night. You're fighting to breathe for hours on end, which puts your body under enormous stress. This triggers sweating, even though you're not aware of the struggle happening whilst you sleep. - Morning headaches
When your brain is starved of oxygen repeatedly throughout the night, it responds with a headache. These typically fade within an hour or so of waking as your oxygen levels return to normal, which is why people often dismiss them as stress or dehydration rather than recognising them as a warning sign. - Dry or sore throat in the morning
Two things cause this. First, your soft palate (the soft tissue at the back of your mouth) flaps around violently all night during snoring, causing repeated trauma to the tissue. Second, you end up breathing through your mouth, either because your nose is blocked or because you physically need to gulp air in to compensate for the obstruction in your throat. Breathing through your mouth all night dries out your saliva, leaving you parched and uncomfortable in the morning. - Heartburn and reflux symptoms
Acid reflux, a feeling of a lump in your throat, constant throat clearing, hoarseness after talking for a while, occasional throat spasms during swallowing. These happen because you're working so hard to breathe against a blocked airway that your abdomen needs to generate extra tension and pressure. This forces stomach contents back up into your throat. Many people are treated for reflux with medication when the real problem is their airway obstruction. - Reduced sex drive
When your body is under constant stress (which it is, fighting to breathe all night), it purposely shuts down non-essential functions. Reproduction is not a priority when your body thinks you're in survival mode. This is the same reason why sleep apnoea can cause infertility in both men and women: reduced sperm production, irregular or absent menstruation, and increased risk of miscarriage. Your body is saying "this is not a safe time to make a baby." - Depression, anxiety, and irritability
Sleep deprivation has a profound effect on mental health. Your brain chemistry changes when you're chronically sleep deprived. Serotonin and dopamine levels drop, making it harder to regulate emotions and maintain a positive mood. You're more likely to snap at loved ones, feel overwhelmed by small problems, and struggle with feelings of hopelessness. Many people are prescribed antidepressants when treating their sleep apnoea would address the root cause.
"I found it impossible to believe that it was normal to feel so tired all the time when I was 'sleeping' for 7-9 hours every night and still not waking up refreshed in the morning."
– Felicity Knapton, Google review
Do These Symptoms Sound Familiar?
If you're recognising yourself in these symptoms, the next step is to complete a proper assessment. Prof Vik Veer uses validated questionnaires to help identify sleep disorders and assess their severity.
Complete our online sleep questionnaires here: Sleep Assessment Questionnaires
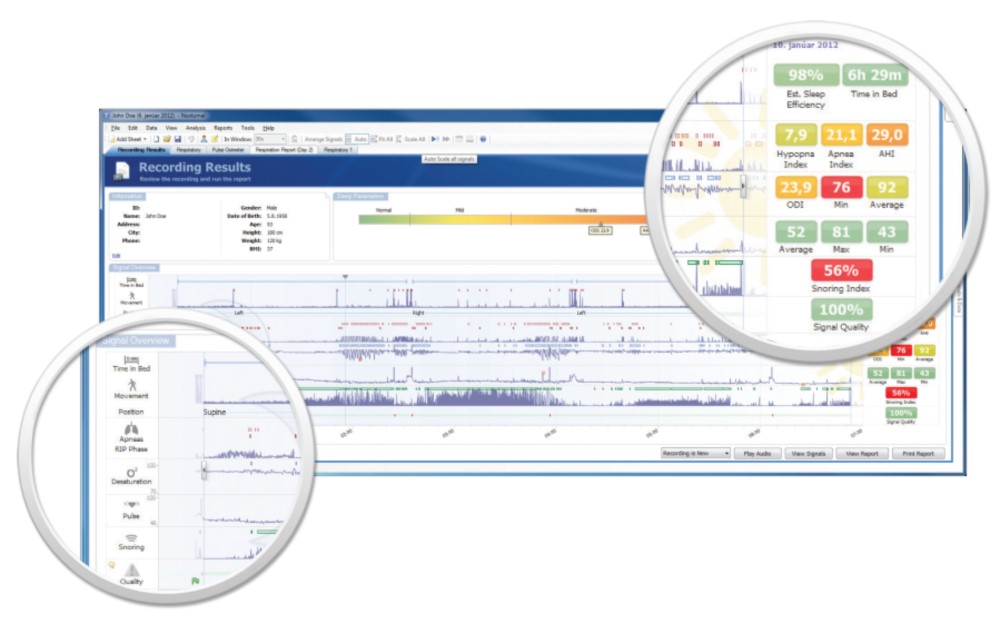
These questionnaires include the Epworth Sleepiness Scale and STOP-BANG assessment, both of which are used internationally to screen for sleep apnoea. They take just a few minutes to complete and can help determine whether you need further investigation with a sleep study.
"After years of getting nowhere fast, I eventually found Dr Veer. From the very first consultation my experience was so refreshing compared to previous doctors. I finally felt understood and listened to."
– Jamie Lewis, Google review
What is a Sleep Study?
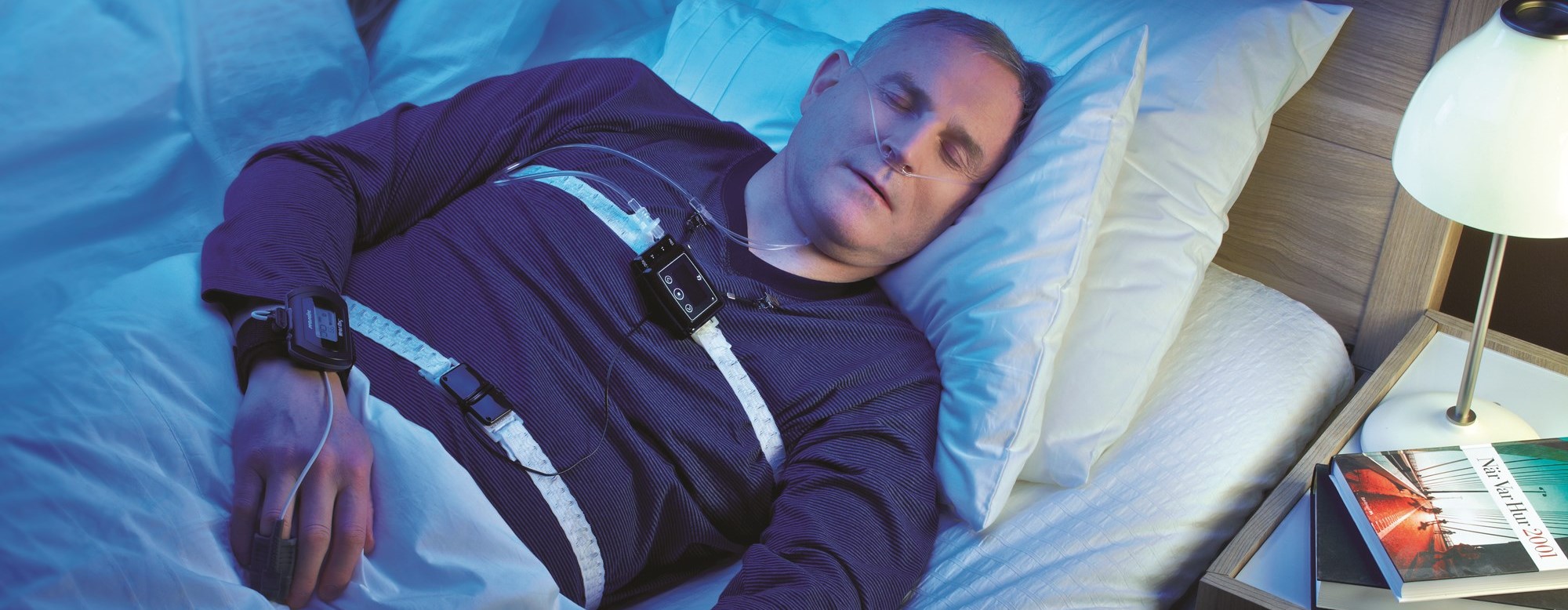
A sleep study, otherwise known as a polysomnography test, is a device that monitors your sleep at night. Most sleep studies are performed to diagnose obstructive sleep apnoea, and occasionally Upper Airways Resistance Syndrome. Sometimes they can be used to diagnose other conditions such as Restless Legs Syndrome or epilepsy.
Sleep studies are performed over one night and can be done either at home or in a hospital. Normally if you're concerned about Obstructive Sleep Apnoea or Upper Airways Resistance Syndrome, then a study performed at home is all you need. If your doctor suggests that you need a sleep study done in a hospital overnight, they will likely also be checking for epilepsy (as they will require a video recording of the sleeping patient). Restless legs syndrome can be diagnosed at home and does not require an inpatient stay, but often a video recording is very useful.
What is it Like to Have a Sleep Study?
A sleep study is a non-invasive test and does not cause any pain or side effects. The device is a smartphone-sized box which is attached via elastic bands that gently wrap around your chest and stomach. There are a number of other cables needed to collect data:
- There is a monitor that sits on your finger which monitors pulse rate and oxygen levels in your blood.
- The elastic straps that go around your chest are there to monitor how hard you are trying to breathe at night.
- The one around your stomach is compared to the one around your chest, and that provides information about people who are struggling to breathe at night (the chest and stomach move in different directions when someone is trying to breathe against a blockage).
- There is sometimes a cable that runs around your nose and monitors the airflow whilst you breathe. This is very important when trying to diagnose Upper Airways Resistance Syndrome.
- There can be a number of other cables that lead to your head or legs to diagnose other conditions.
"Having suffered from severe disruptive sleep apnoea with a severity that was off the Epworth scale, my experience with Mr. Vik Veer has been truly transformative. The results have been nothing short of remarkable."
– Raj Patwal, Google review
What is Pulse Oximetry?
Pulse oximetry is just the device that sits on your finger at night, monitoring heart rate and oxygen levels in the blood. Prof Vik Veer does not recommend the use of these devices alone as they are unable to detect most problems during sleep. It will only pick up very obvious severe sleep apnoea, but in Prof Vik Veer's experience it misses significant problems with sleep disordered breathing.
Prof Vik Veer has met a number of people who have had a pulse oximetry test (which is mainly used by respiratory teams who provide CPAP), who were then told that they have no problem after the test. When they go on to have a proper sleep study, they find out that in fact they have a treatable sleep disorder which helps them with their tiredness and other symptoms. If you know you will only accept CPAP as a treatment option, then a pulse oximetry would be a reasonable choice.

Pulse oximetry is often used for children in the NHS to work out if they should undergo an adenotonsillectomy to solve their sleep apnoea problem. Prof Vik Veer still advocates a proper sleep study even in children.
How Can I Get a Sleep Study Done?
Prof Vik Veer provides a courier service where a state-of-the-art sleep study machine is sent directly to your home or workplace. You would then use the device that night in the comfort of your own bed, and then the courier will return the next day to pick up the device. This avoids having to travel into central London to pick up a device and return it by hand the next day. Because of the courier, this sleep study option is now a national service. Now anyone in the country is able to have a sleep study done whenever they wish.
To get the results, you may want to have a formal report written for you by Prof Vik Veer, or if you prefer, you can visit Prof Vik Veer in his London clinics to discuss the results face-to-face.
If you would like more information or to book in a sleep study, please contact Prof Vik Veer via his team of secretaries:
Private secretary: 0207 458 4584
Email: Secretary@Consultant-Surgeon.co.uk
"Dr Veer has helped me over the last few months identify my sleep apnoea with a home sleep study and endoscopy. My AHI was 24 prior to using CPAP and 15 after using. After using the techniques he recommended, it has fallen to 1!"
– Peter Hurley, Google review
Treatment for OSA
Prof Vik Veer has the largest practice in the country for treating obstructive sleep apnoea with surgery. He operates on approximately 260 patients a year specifically for snoring and sleep apnoea. He is the most experienced full-time NHS consultant who has been employed specifically to treat sleep apnoea with surgery. He is also the only surgeon in the country fully funded on the NHS to carry out this work.
There are different types of treatment for obstructive sleep apnoea. Some require surgery, and some do not:
- Continuous Positive Airways Pressure Mask (CPAP)
 This is when a mask is fitted to your face each night to drive air into your lungs whilst you sleep. This is an excellent treatment choice for those who can tolerate it. Unfortunately, about 50% stop using it after the first week, and 83% stop using CPAP long-term (Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008 Feb 15;5(2):173-8).
This is when a mask is fitted to your face each night to drive air into your lungs whilst you sleep. This is an excellent treatment choice for those who can tolerate it. Unfortunately, about 50% stop using it after the first week, and 83% stop using CPAP long-term (Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008 Feb 15;5(2):173-8).
Most patients have difficulty coping with the feeling of claustrophobia and finding that the device itself wakes them up at night. Minimum compliance with CPAP is defined as using it for 4 hours a night 70% of the time. However, for CPAP to be effective, you should use it every night for at least 7.5 hours; otherwise, you'll still suffer with the complications of sleep apnoea. For those patients that only manage to use it for 4 hours a night 70% of the time, research has shown that the AHI in these patients is still about 11.91 on average, which is still defined as sleep apnoea (Stuck BA, Leitzbach S, Maurer JT. Effects of continuous positive airway pressure on apnoea-hypopnoea index in obstructive sleep apnoea based on long-term compliance. Sleep Breath. 2012 Jun;16(2):467-71).
In some European countries, patients are warned that if they don't use the CPAP device, their driving licences will be confiscated. This is not the case in the UK at the moment. Please see the current DVLA page on sleep apnoea.
The main advantage of CPAP is that there are very few side effects if you can tolerate the device. Also, using CPAP before undergoing surgery makes the operation much safer, and Prof Vik Veer will explain that if using CPAP is a possibility, patients should continue CPAP even during surgical treatments. The plan would be to slowly come off CPAP and sleep without it once all the treatment is completed. - Mandibular Advancement Devices
These are basically gum guard-like devices that bring your lower jaw forward. If your tongue causes most of your obstruction during sleep, then this should allow you to breathe better at night. There are again some difficulties with being able to tolerate this device in your mouth all night, and some patients complain of tooth loosening and sore jaw joints in the mornings. These devices may be used with CPAP as well. - Myofunctional Therapy
This is a useful new specialist therapy which is increasingly used as a treatment for snoring and sleep apnoea. It is often used in addition to other therapies, but because of the low risk, it can be used for all patients. - Surgery for Snoring and Obstructive Sleep Apnoea
If patients cannot tolerate or dislike the idea of CPAP or Mandibular Advancement Devices, then another option is surgery.
From the back of the nose to the voice box, there are many different problems in the throat that can cause snoring or sleep apnoea. Therefore, there are many different operations, and every patient is different. No one has the same problem, and therefore there is no one operation that fixes everyone. In the past, surgeons used one operation to try and cure sleep apnoea, but because it was only the correct operation for a small percentage of patients, only a few people gained benefit from it. Using modern surgical techniques, we are now able to determine what is causing the problem in each case. Using this information, Prof Vik Veer is able to select the correct operation for each patient. - Drug Induced Sleep Endoscopy (DISE)
This is when a very small amount of anaesthetic is given to drift a patient off to sleep. At the same time, a tiny fibreoptic telescope is used to visualise the throat whilst the patient is asleep. The whole procedure takes about 10 minutes or so, and the risk of complications is extremely low.
Currently, DISE is the only way to find out where the snoring noise is coming from and what is causing the obstruction in the upper airway. Unfortunately, all the other techniques for determining the cause of obstruction only really tell you the approximate anatomical level rather than the actual problem. For example, a large uvula, a lateral pharyngeal wall collapse, a tongue base obstruction, tonsillar obstruction, or an epiglottis trapdoor problem all occur at roughly the same level. At this level, they can all cause problems simultaneously and to a different degree in each individual. That is why Prof Vik Veer uses DISE to identify the actual problem and know how to treat it. The quality of DISE recordings have improved considerably in recent years with newer techniques for this investigation.
Prof Vik Veer has spoken internationally about DISE and has introduced a new classification system for its use. DISE is a difficult technique, and Prof Vik Veer has conducted an international survey on DISE and found that the understanding of this procedure in the UK is poor. He is a world expert in this field and will be happy to discuss this technique in more detail with you if you wish.
There are a multitude of operations that can help patients with snoring and sleep apnoea, and they range from the minimally invasive to the more extensive. A brief outline of these operations is provided below: - Nasal Operations
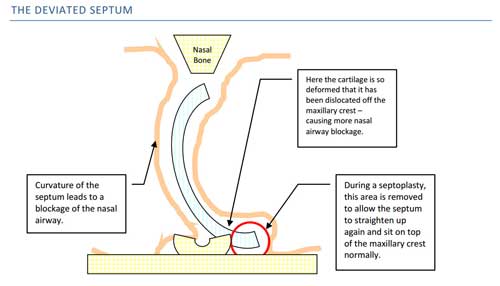
Improving the flow of air through the nose does not actually improve snoring or obstructive sleep apnoea directly, and in some cases it actually makes snoring worse. This is because even though you now are able to breathe through your nose, it does not necessarily mean that you will automatically start breathing through your nose during sleep. Breathing through the mouth becomes a habit for people, and so it is unlikely that you will preferentially use the nose to breathe even after surgery. In these cases, using a chin strap (a device to close the mouth at night) is enough to slowly convince you to breathe through the nose and hopefully reduce the volume of snoring to a socially acceptable level. Once the patient has become accustomed to breathing through the nose again during sleep, he or she should be able to stop using the chin strap and carry on without it. - Septoplasty & Turbinate Reduction
There are many different operations for the nose. Some operations (such as turbinate reduction) can be done under local anaesthetic and have very few complications. Other operations, such as a septoplasty (where the central partition of the nose called the septum is straightened up so you can breathe equally on both sides) and polypectomy (where polyps are removed from the nose to help breathe past them), can take longer to perform and will probably require a few days off work. Choosing the correct operation is a difficult balance and sometimes can only be decided during the operation itself. Most of the time, Prof Vik Veer will choose the least invasive option to help patients breathe better. - Palatal Operations
These operations include any operation involving the palate or uvula (the dangly thing at the back of your throat). This includes using a laser or other techniques to stiffen or reduce the size of the palate. In the past, surgeons only used these operations to try and treat Obstructive Sleep Apnoea. This was always bound to fail as the palate is a flap and can close the entrance to the nose OR mouth. What the palate cannot do is block the nose AND the mouth at the same time. So if the palate is blocking the nose, the patient will just open their mouth and breathe through their mouth instead, or vice versa. This will lead to snoring certainly, but the patient will still be able to breathe, meaning that they cannot get Obstructive Sleep Apnoea.
Occasionally the uvula may be involved in blocking the airway. The uvula can drop down behind the tongue where the majority of obstruction in sleep apnoea occurs. The uvula may block off the last 5-10% of an already severely constricted airway. So in the past, when surgeons just operated on the palate, removing the uvula (which is a part of these palatal operations) only opens a small amount of the airway. This is why some sleep apnoea patients did initially get better after this operation, but normally this effect did not last for long. This led to recurrence of problems, particularly in the long term.
With newer techniques recently developed, we are able to identify these issues and choose the correct operation for each patient.
In most cases, sleep apnoea patients need very little done to the palate, which means the pain from this operation is greatly reduced. Most people who snore without obstructive sleep apnoea have a problem with their palate. There are now various techniques to scar and stiffen the palate to make it more rigid and tight. This stops it vibrating so much and therefore reduces the noise that it generates. Some operations cause minimal pain but may take longer to have an effect. Prof Vik Veer will be happy to discuss the options with you as he has taught on international courses about these techniques. - Large Tonsils
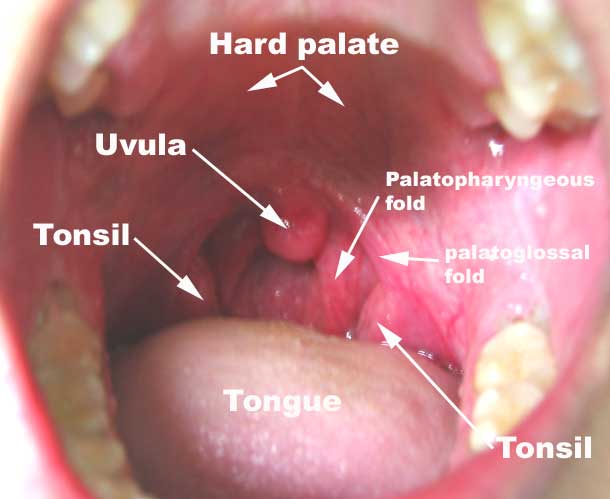 Tonsils can obstruct the airway by meeting together in the middle and not allowing any air to pass. Sometimes, even though tonsils look small inside the mouth, they can still have a large component at the back of the throat that can still cause significant problems breathing. So using DISE certainly helps in the investigation of these patients to decide if a tonsillectomy is required.
Tonsils can obstruct the airway by meeting together in the middle and not allowing any air to pass. Sometimes, even though tonsils look small inside the mouth, they can still have a large component at the back of the throat that can still cause significant problems breathing. So using DISE certainly helps in the investigation of these patients to decide if a tonsillectomy is required.
A tonsillectomy is a relatively quick operation, taking less than 5-10 minutes on average. There are a number of ways of removing tonsils, and more information about this can be found on the tonsillectomy page on this website. In brief, for snoring and sleep apnoea patients, Prof Vik Veer normally uses a cold steel intracapsular tonsillectomy technique for most patients. It isn't possible to use a tonsillotomy approach in sleep patients as it still leaves tonsillar tissue behind, and that can still lead to obstructive sleep apnoea and snoring. In children, an intracapsular tonsillotomy (coblation) approach is probably adequate in most cases. Discussing the pros and cons of different types of tonsil operations is a difficult balance, and Prof Vik Veer will be happy to discuss this with you and explain it all. - Lateral Pharyngeal Wall Collapse
In some patients (particularly in those with sleep apnoea and loud snoring), the lateral pharyngeal wall collapses down and obstructs the airway. This is the back wall of the throat you can see behind the tonsils and behind the uvula. In some severe cases, you can even see a bulging of the tissue here behind the tonsils, which Prof Vik Veer calls 'lateral wall cushions', which is one of the signs that this area is a problem.
The back wall of the throat collapses down towards the back of the tongue and the back of the palate, sometimes completely blocking off the throat and causing Obstructive Sleep Apnoea. It is a difficult area to treat, and only a minority of surgeons in the world actively operate here.
Expansion Sphincter Pharyngoplasty is one of the operations that is used to remedy this problem, and there are several modifications to the original described technique. In short, it uses some of the muscles in the back of the throat and redirects them. By attaching these muscles in different locations, the airway can be forced open rather than collapse upon itself. It is a powerful technique in the correct patients, and Prof Vik Veer has had complete cures (AHI less than 5) in some extremely severe sleep apnoea patients (AHI > 100!) with this operation.
There are a few other operations that can be used to treat this problem, many of these are being developed by Prof Vik Veer. - Tongue Base Operations
The tongue is a common reason why people have Obstructive Sleep Apnoea, and rarely snoring noise comes from here. The tongue falls back and blocks the throat, stopping breathing.
The tongue is extremely difficult to operate on, and therefore Prof Vik Veer has experience with a number of techniques to use so that he can individualise care for each patient. The least painful operation is radiofrequency ablation of the tongue base, which stiffens and shrinks this area so patients can breathe past the obstruction. Coblation and robotic surgery of the tongue base are other techniques which reduce the volume of the tongue so that it doesn't obstruct breathing.
 There are also a number of nerve implants that can be used in sleep apnoea. Prof Vik Veer provides the Inspire and Genio Nyxoah devices for sleep apnoea.
There are also a number of nerve implants that can be used in sleep apnoea. Prof Vik Veer provides the Inspire and Genio Nyxoah devices for sleep apnoea.
Prof Vik Veer is also leading research into a new implantable device that will be inserted into the tongue to stimulate it so that it doesn't block the throat. This operation will be the first of its kind in the United Kingdom and should be available once the results are verified. - Laryngeal Obstruction
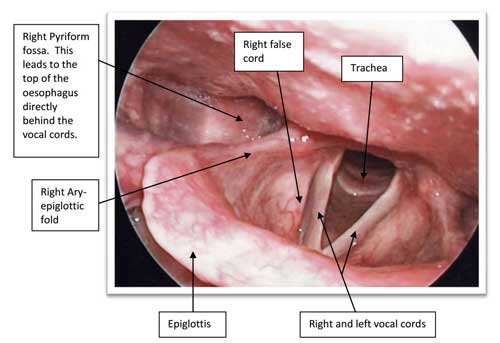 There are a number of problems that may affect the larynx (also known as the voice box), and the epiglottic trapdoor is the most common of these. The epiglottis is used to divert food away from the voice box during swallowing so that food doesn't go down the wrong way. In some patients, the epiglottis collapses back into the voice box during breathing, which completely blocks off the ability to breathe. This is one of the reasons why CPAP actually makes these patients worse rather than better. There are a number of other different problems of the larynx that can make breathing more difficult.
There are a number of problems that may affect the larynx (also known as the voice box), and the epiglottic trapdoor is the most common of these. The epiglottis is used to divert food away from the voice box during swallowing so that food doesn't go down the wrong way. In some patients, the epiglottis collapses back into the voice box during breathing, which completely blocks off the ability to breathe. This is one of the reasons why CPAP actually makes these patients worse rather than better. There are a number of other different problems of the larynx that can make breathing more difficult.
These are the very basics of the surgical options for snoring and sleep apnoea. Obviously, there are a number of modifications and subtleties that are not included here. Most of the differences occur when a number of different obstructive problems occur simultaneously. In this situation, individualised treatment is needed, and Prof Vik Veer will explain this to you in detail.
"I've been seeing Mr Veer for severe sleep apnoea for approximately 18 months. I am pleased to say I'm off the CPAP machine and breathing and sleeping is again a pleasure at night. Mr Veer has changed my life."
– Jeremy Rideout, Google review
"Dr Vic Veer absolutely saved my life. I had very obstructive sleep apnoea with serious effects, and Dr Vic Veer performed 4 very invasive operations on my palate, mouth, throat and neck, basically reconstructing my throat and airways, enabling me to breathe correctly and curing me of the condition."
– Wesley Burne, Google review
Read more
This is an overview of the treatment of snoring and sleep apnoea. If you would like to know more, please use the links on this page to understand better what the treatment options for these conditions are.
If you would like more information or to book in a sleep study please contact Prof Vik Veer via his team of secretaries:
Private secretary: 0207 458 4584
Contact Mr Vik Veer
Alternatively contact Mr Vik Veer and his secretarial staff directly using the form below.